Humans are wired uniquely. As the saying goes, “Different strokes for different folks”—even in patient teaching.
Adapting to patient learning styles makes patients feel heard. And showing empathy is important in a clinician-patient relationship.
Until the mid-20th century, doctors dominated the decision-making process. But since then, the relationship between physicians and patients has transitioned to something more like a partnership. Patients are now considered active participants in their health.
Easy-to-understand patient education infographics that match patient learning styles are critical to educating patients and helping them grasp information immediately.
If you’re looking for educational materials, you can start by matching patient learning styles to infographics with Venngage.
But first, you need to understand patient learning styles.
In this article, we dive deep into types of learning styles, benefits of patient teaching, and various teaching modalities that match learning styles.
Click to jump ahead:
- Why are patient learning styles so important?
- 4 main patient learning styles
- What does patient teaching mean?
- Why is patient teaching important?
- Patient teaching strategies
- Guidelines for developing patient education materials
- How do you know a patient is ready to learn?
- What are some of the barriers that affect a patient’s ability to learn?
- Patient teaching FAQ
Why are patient learning styles so important?
Learning is not a one-size-fits-all approach.
Research has continued to provide evidence that patient-specific teachings are better than generalized teaching.
One popular explanation for why patient learning styles are important is the meshing hypothesis.
According to the meshing hypothesis, the best learning happens when the format of teaching matches the preferences of the learner.
There are various learning style models, including Kolb, Gregorc, Felder–Silverman, VARK, and Dunn and Dunn. Below, we highlight the VARK model.
In 1992, a study by Neil D. Fleming and Coleen E. Mills led to the popularization of the “VARK model,” which describes four main learning styles.
4 main patient learning styles (according to the VARK model)
1. Visual
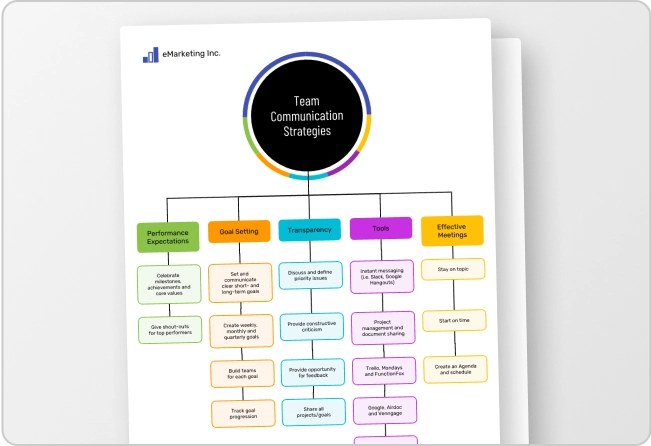
Patients who learn visually prefer figures, pictures, and symbolic tools like graphs, flowcharts, hierarchies, and models. They generally have a good sense of balance and alignment, organization, and color orientation. Visual patients benefit greatly from health infographics.
For example, this recommended vaccinations timeline appeals to visual learners because of the use of a bright color palette, bold headings, and modern font that make the infographic pop off the page.
2. Aural/Auditory
Patients who are auditory learners prefer to learn by listening. Aural learners benefit from audiotapes, podcasts, YouTube videos, or videotapes.
3. Reading/Writing
Patients who learn through reading or writing love the printed word. They prefer resources like textbooks, journal publications, doctor’s notes, online articles, blogs, and other written texts.
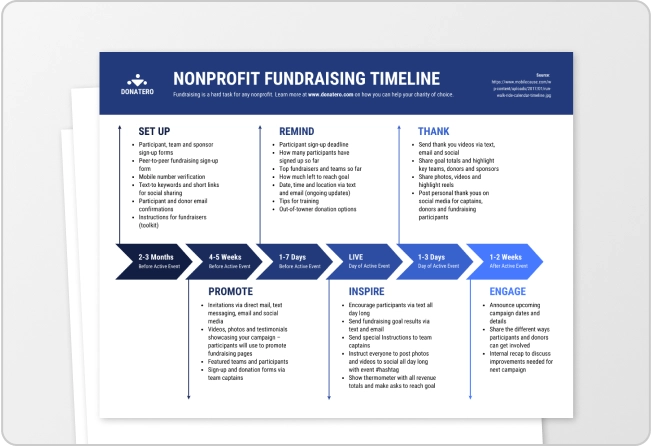
This infographic below appeals to patients who love the printed word. You can see well-defined steps and each step contains a sub-title with a full description of actions to take.
4. Kinesthetic
Patients who are kinesthetic learners get their education from experience.
Authors William A. Drago and Richard J. Wagner describe kinesthetic learners as people who “have high energy and prefer to apply touch, movement, and interaction to their environment.”
What about multimodal learners?
Individuals typically do not stick to one learning style.
Just as in most things in life, people can exhibit “multimodal” traits. Multimodal learning involves the use of a combination of senses during learning.
Patients who do not have a strong preference towards one particular learning style may fall in this category.
Some multimodal learners are flexible: they’re comfortable with multiple learning styles and can switch from one learning mode to the next to suit the situation they’re dealing with.
Others are not as much: they need input or output from all their preferred learning styles before they can make a decision or understand everything.
What does patient teaching mean?
We will define patient teaching by going back to the Latin root word for doctor, “docere.”
In Latin, docere means “to teach.” At the core of being a physician or health provider is the ability to teach your patients so that they can have the best health outcomes.
Education is an interactive process in which learning takes place. Patient teaching is a specific type of education in which health professionals help patients and their caregivers learn about how to improve their health and be involved in their ongoing care and treatment.
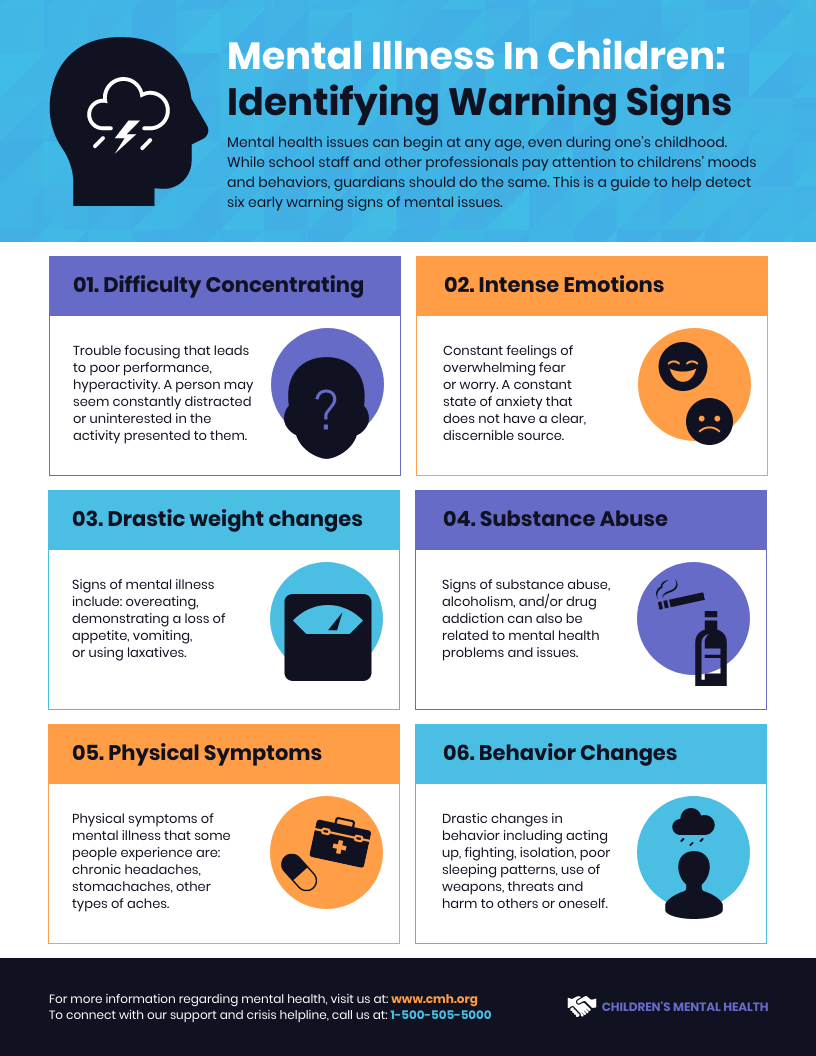
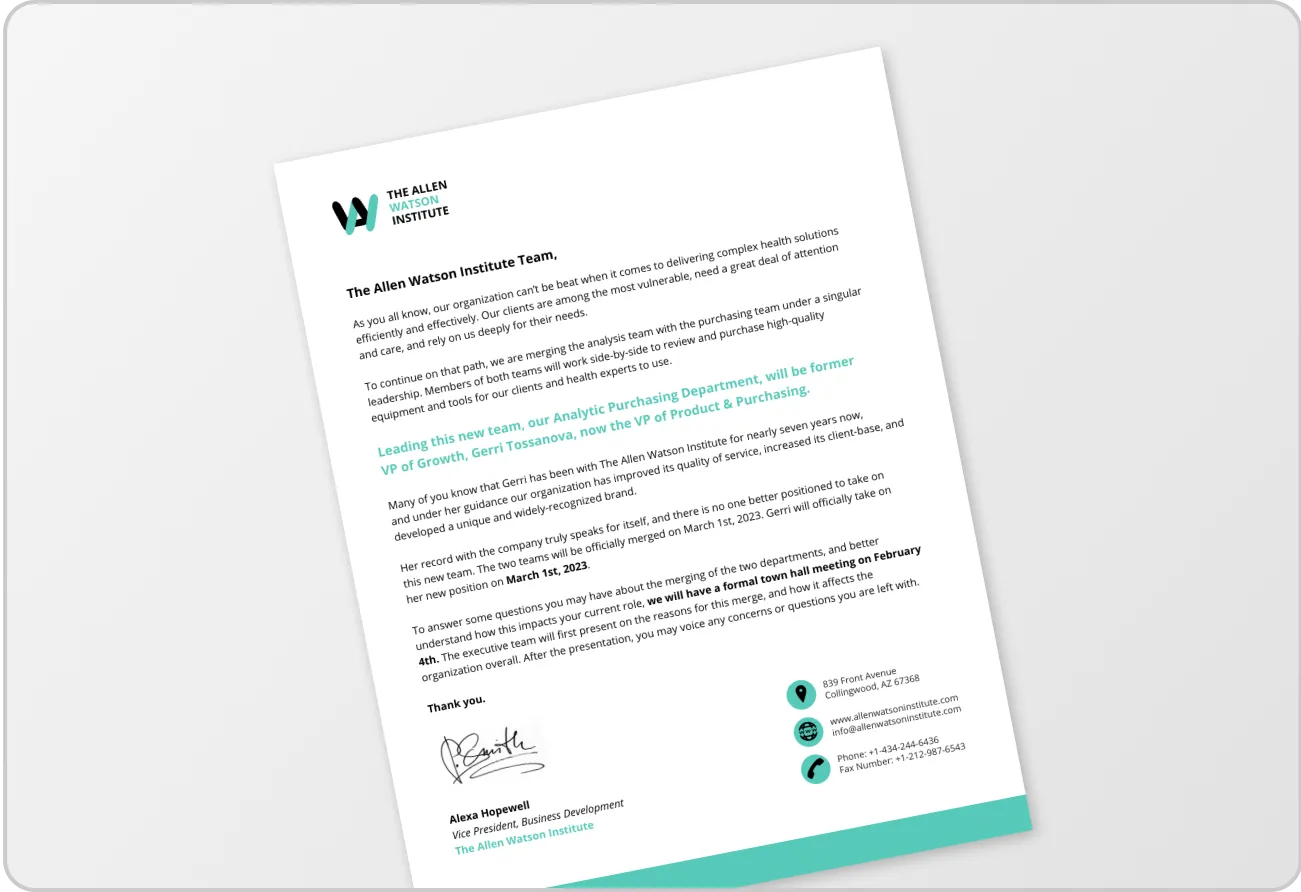
The infographic below is a great example of patient teaching. Most patients do not know the major signs and symptoms of medical conditions off the top of their heads. The pictures and drawings quickly illustrate the words and patients can catch on easily.
Why is patient teaching important?
There are tons of research spanning decades portraying the importance of patient teaching.
Let’s go over some reasons why patient teaching is important.
1. Patient teaching decreases anxiety
There is evidence that uncertainty results in anxiety and early warnings decrease anxiety. If you know an event is coming up on your calendar, you can plan ahead. However, if you can’t predict that an event will have a positive outcome, you may become anxious.
According to neuroscience experts Dan W. Grupe and Jack B. Nitschke,
The ability to use past experiences and information about our current state and environment to predict the future allows us to increase the odds of desired outcomes while avoiding or bracing ourselves for future adversity. This ability is directly related to our level of certainty regarding future events – how likely they are, when they will occur, and what they will be like. Uncertainty diminishes how efficiently and effectively we can prepare for the future, and thus contributes to anxiety.
Patient teaching alleviates anxiety. Clinicians can help patients understand warning signs and complications, which means that patients will know exactly what to look out for.
For example, in this Early Warning Signs of Mental Health Illness infographic, the eye-catching images quickly illustrate signs that patients should talk to their doctor about.
2. Patient teaching increases adherence and compliance
When clinicians take time to teach, patients become more comfortable with following therapy instructions.
A patient who understands the “why” is more inclined to follow the doctor’s orders. Healthcare providers should focus on communicating the why’s through various patient teaching techniques.
For example, this patient infographic below clearly states, “If you skip, change, or ignore your medicine, it can be bad for your health.” Physicians can use this infographic to teach patients about the benefits of adherence and compliance.
3. Patient teaching increases knowledge
One aim of patient teaching is to increase patients’ understanding of medical conditions. Patient teaching also improves understanding of health-promoting behaviors.
Armed with the right knowledge, patients can improve their attitudes toward preventive health and use the correct methods and procedures when caring for themselves at home.
Home health teachings are great for educating patients about how to maintain their health at home. An example is this infographic that teaches patients on how to prevent catching and spreading the coronavirus.
4. Patient teaching increases satisfaction
The doctor-patient interaction is probably the most important factor that affects patient satisfaction.
Interpersonal skills—how clinicians communicate and interact with patients—come in handy during patient teaching. Patients often want health providers who are empathetic and understand their specific needs.
The infographic below helps patients compare three different medical aid plans. This is an empathetic teaching tool as there is the understanding that priorities are different for each patient.
5. Patient teaching reduces hospital re-admission rates
About one in five patients discharged from hospitals have complications within 30 days. This results in visits to the emergency room (ER) or re-admission.
One of the reasons for rehospitalization is low health literacy. According to Health.gov, “Literacy skills affect how people find, understand, and use information on the web. Users may get distracted easily, give up quickly, and struggle with dense text and complex navigation.”
If patients don’t understand their illness or how to maintain their treatment, they won’t know how to care for themselves. This increases the risk for hospital readmission.
According to the Centers for Disease and Control (CDC), patients with low health literacy are more likely to visit an emergency room, have more hospital stays, not follow treatment plans, and have higher mortality rates.
Patient teaching strategies
Various sources recommend using a combination of multiple clinician patient teaching and nursing teaching strategies for patients.
Providing patient education materials in various modes reinforces teaching.
Patient teaching methods involve using the following tools:
- Written materials
- Graphics (including infographics)
- Posters or charts
- Audiotapes/Podcasts
- YouTube videos
- Videotapes or DVDs
- PowerPoint presentations
- Demonstration using models or props
- Traditional lectures or group classes
- Verbal teaching
- Discussions
This First Trimester infographic below combines different patient teaching strategies.
You can see how graphics are used in combination with words. Also, this infographic can be enlarged and used as a poster or prop during a traditional lecture, in a doctor’s office, or as a nurse teaching topic.
In one study, verbal teaching and discussions were the least effective teaching strategies. The authors recommend that verbal teaching should be used in combination with other teaching strategies and not alone.
Also, cognitive research shows that the human brain processes text/audio and visual information in two separate channels. The authors of Seven practical principles for improving patient education: Evidence-based ideas from cognition science wrote about a theory called the Dual code.
“Dual code theory suggests that humans have separate cognitive ‘channels’ for text/audio information versus visual information. By constructing educational messages that take advantage of both channels simultaneously, information uptake may be improved.”
For example, in addition to verbal teaching and discussing patients’ eligibility for telemedicine, doctors and nurses can provide patients with this simple infographic, either printed so they can take it home or available on a website so they can download and save for future reference.
Guidelines for developing patient education materials
To get all the benefits of patient teaching, you need to follow proven guidelines when developing effective patient education strategies and materials.
Here are some guidelines on how to teach patients suggested by the American Academy of Ambulatory Care Nursing (AACN):
- Use visuals frequently to show anatomical features.
When describing a disorder or problem that relates to a part of the body, your patients will have a better understanding when you use anatomical illustrations in your descriptions.
- Use plain language.
Write in language that patients use daily. Avoid scientific jargon. Also, define any terms that may be difficult for patients.
- Create written materials at the third to fifth-grade level.
The more simple your text, the more your patients will grasp the subject matter. Avoid technical jargon to avoid patient confusion.
Related: How to Simplify Technical Jargon for Healthcare Patient Education Materials and Infographics
- Sentences should be short (10 words or less).
It’s easy to lose track when reading long-winded printed materials. Keep your sentences short and sweet so that your patients can follow along.
- Keep paragraphs between two and three sentences with one key point per paragraph.
Give patients the main idea right away.
- Use bullet points with “must know” information.
Summarize the key takeaway message for patients in bullet points.
- Insert visual language.
Use phrases such as “runny nose” and “redness.” Patients need to visualize what you’re describing in everyday language.
- Explain measurements.
Limit your use of scientific measurement descriptions. For example, write “pain that lasts more than 30 minutes.”
- Be aware of language, customs, and values.
You need to consciously describe your content in a culturally sensitive way.
- Use wide margins and leave white space between sections.
This makes your content easy to read.
We like this infographic below because it uses drawings of anatomical features and plain language to illustrate what the virus that causes COVID-19 does when it enters your body. The illustrations can help patients picture what’s going on inside their bodies.
How do you know a patient is ready to learn?
Before you teach a patient, assess whether they are ready to learn.
The Agency for Healthcare Research and Quality (AHRQ).
Next, ask if your patient is ready to learn. Some patients want you to get right to it, but others may have distractors in their life that hinder learning.
After checking readiness, find out what your patient’s learning style is. Next, agree with your patient on realistic learning objectives.
After these checks, your patient may be ready to learn.
What are some barriers that affect a patient’s ability to learn?
Some factors that can hinder a patient’s ability to learn include:
- Fear. Your patient may need to overcome fear before being open to teaching.
- Capacity to handle information. Individuals have different limits when it comes to handling sensitive information. Give your patient only the amount of information they can handle at a time.
- Receptive to teaching. Some patients embrace learning. Others need nudging and encouragement from their clinicians.
- Lack of time. Due to strict scheduling, physicians often do not have enough time to educate patients.
- Health status. Adjust your education plan based on the level of your patient’s health status.
- Lack of knowledge and skill level of health providers. Clinicians, nurses, and health educators need to keep updating their training on patient education.
- Rising healthcare costs. In trying to save costs, patients tend to spend less time in the hospital before procedures such as surgery. Therefore, nurses and physicians have less time to teach patients about such procedures.
You can note down these points or save this infographic to help with your patient teaching:
Patient teaching FAQ
Who provides patient education?
Effective patient education can be provided by healthcare professionals and experts who have comprehensive skills.
Here are some examples of healthcare professionals involved in providing patient education:
- Physicians
- Nurses
- Clinical instructors
- Lead faculty and teachers
What do you teach a patient?
Healthcare practitioners teach patients various topics. Here are some patient teaching examples:
- What medical conditions mean
- The risks of medical conditions
- Treatment options
- How to take medications
- How to prevent disease or injury
- How to reduce complications
- How to make lifestyle modifications for better health outcomes
What is patient teaching in nursing?
Nursing is the largest healthcare profession in the US, with more than 3.8 million registered nurses. Therefore, nurses are critical in patient teaching.
Nursing teaching happens while taking care of hospitalized patients and during discharge planning.
Nurses create nursing teaching plans, talk to patients, find out how they’re doing, and answer questions. During discharge, nurses teach patients what to do when they get back home.
The discharge planning nurse is responsible for demonstrating simple procedures that the patient needs to follow. For example, nursing patient teaching may include medication teaching plans, how to properly wrap a wound, or how to read a glucometer. Nurses also cover the types of complications that can occur at home and warning signs.
In summary: Patients learn better when infographics are matched to patient learning styles
Infographics are perfect for visually representing medical information. You can use infographics to simplify complex terms by using plain language, figures, pictures, and symbolic tools like graphs, flowcharts, hierarchies, and models.
Due to their visual nature, infographics cater more to people with visual and reading/writing styles. However, for the best learning outcomes, patient educators should combine different methods that cater to people with various learning styles.
You can start matching patient learning styles with educational content by using Venngage’s easy-to-use editor and our various fully customizable healthcare templates, and within minutes you will have effective tools for patient teaching.